Ear infections 101
About 25% of infants have at least one ear infection in the first year of life. They are painful, and they are frustrating.
Today’s article covers why infections happen, what cause them, and which kids are at highest risk for them.
Check out this article for the practical tips: how to tell if your child has one, when to call your doctor, and treatment/management.
And check out the guides section for a free download on tips and tricks to try at home!
Ear infections: the basics
Types of ear infections
There are two main types of ear infections.
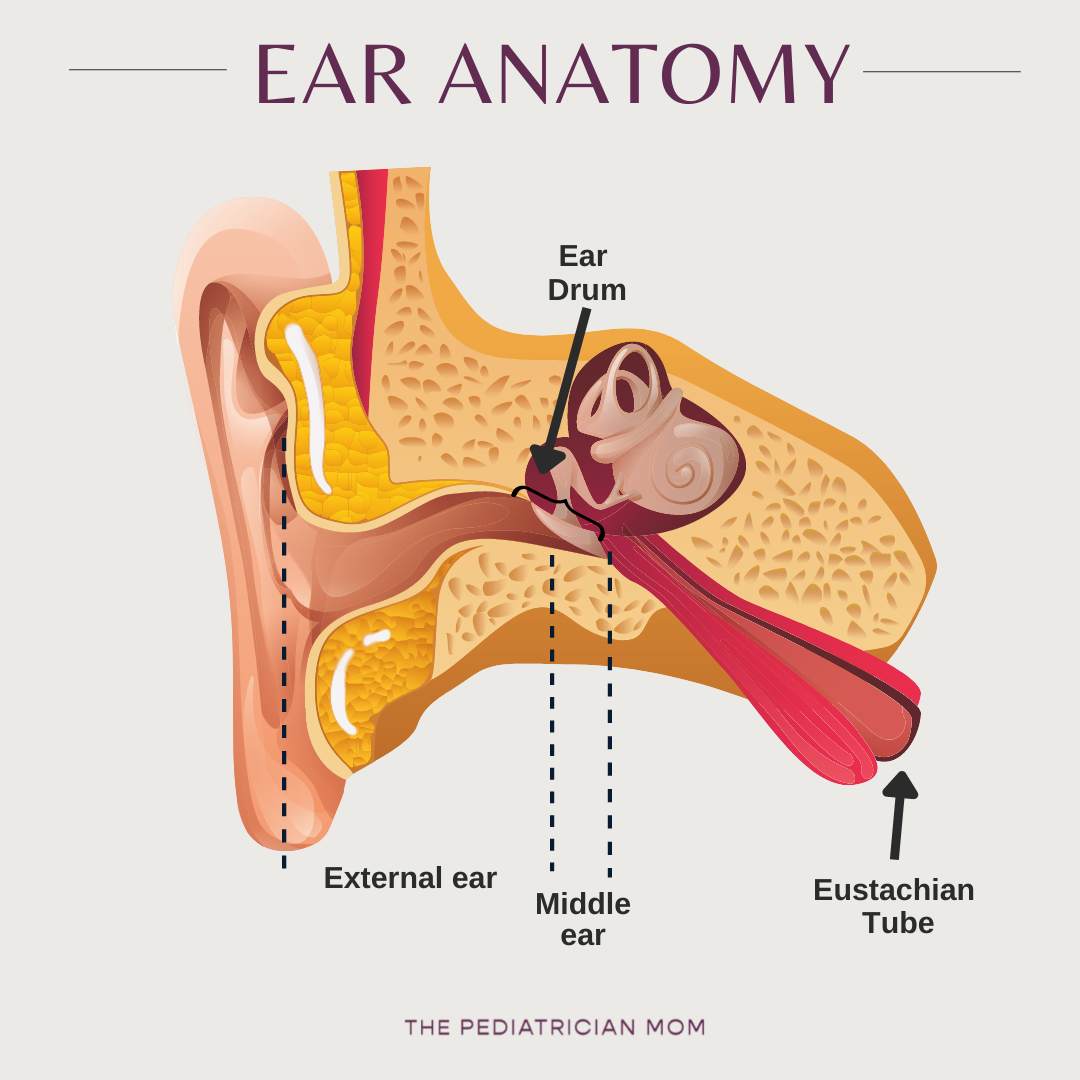
Otitis externa: an infection of the external ear. Swimmers ear is an example of this, and it is less common in infants and toddlers.
Otitis media: an infection of the middle ear. These are far more common in infants and toddlers.
The two sections are separated from each other by the ear drum (or tympanic membrane).
Ear anatomy basics
The ear canals and the nose are connected by the Eustachian tube. The eustachian tubes regulate pressure in the inner ear and act as a channel for drainage. When we swallow/chew, they normally open and allow pressure to be released. If they are blocked then pressure can build up and cause pain.
In adults, eustachian tubes are longer and point downwards, which makes them more effective at draining fluid, but in children (and especially young babies) they are thinner, shorter, more floppy, and more horizontal.
How do ear infections happen?
Irritation and inflammation occur in the nose or the Eustachian tube itself. This can happen because of an upper respiratory infection, allergies, etc. Any infection in the nose is more easily transmitted up to the ears in kids because of the differences in anatomy.
In the nose/throat, this leads to mucus production.
In the eustachian tube, this leads to swelling and fluid buildup (called an effusion).
Because the eustachian tube is narrow, swelling impairs drainage further.
Simply having fluid there can lead to pain because it leads to bulging of the ear drum but this does not necessarily mean that there is a bacterial infection that needs antibiotics.
But germs also like stagnant fluid. Any fluid sitting there is at high risk of getting infected (this is why we sometimes see secondary bacterial ear infections at the tail-end of viral upper respiratory infections).
In some cases, the pressure buildup can lead to perforation or rupture of the ear drum.
Causes of middle ear infections
Common bacterial causes of ear infections are S.pneumoniae, H.influenzae, M.catarrhalis. They can be caused by other bacteria too as well as by viruses and (more rarely) fungi.
Did you know? Once routine immunizations against S.pneumo and H.flu became part of the infant vaccine schedule, the rate of middle ear infections substantially decreased.
Risk factors for ear infections:
Age (infants between 6-12 months are at highest risk)
Anatomy
Family history, especially amongst siblings
Exposures: daycare, second-hand smoke, pollution, pacifiers
Upper respiratory infections
Is there anything I can do to prevent them?
Unfortunately, in many cases ear infections are a result of anatomy, genetics and (sometimes) bad luck. Minimizing risk factors (listed above) is helpful, but it cannot guarantee that your child will avoid infections entirely.
In general, the most helpful thing to do is to try to clear out nasal secretions because it might prevent the inflammation and fluid reaching the Eustachian tubes. The best way to do this is using nasal saline/steam and suction, such as with the Nose Frida.
Complications of ear infections:
Recurrent ear infections can cause persistent fluid in the middle ear, or scarring of the ear drum, which can then lead to hearing loss.
Ear infections can also spread into the bone, the sinuses, and even the brain. This is very rare.
The ear drum can perforate if the pressure builds up enough. This actually relieves the pain, but is obviously not ideal. The good news is that in most cases, this will heal on its own.
What you can try at home
Check out a free handout in the guides section with some tips.