What to do if your child tests positive for COVID-19
What do you do if your child tests positive for Covid? A helpful guide for parents.
Keep in mind that this information is not a substitute for an in-person medical evaluation from your healthcare provider. Although it can be helpful, it should never be your only source of information. Always touch base with your child’s pediatrician or a qualified healthcare provider to get specific instructions for your child.
Another wave
All signs indicate that we are seeing another wave, although surveillance is more challenging than it has been in the past. I suspect official tracking (which is weaker than it was in the past) is also undercounting the case numbers based on the fact that most people use home tests, which are not reported.
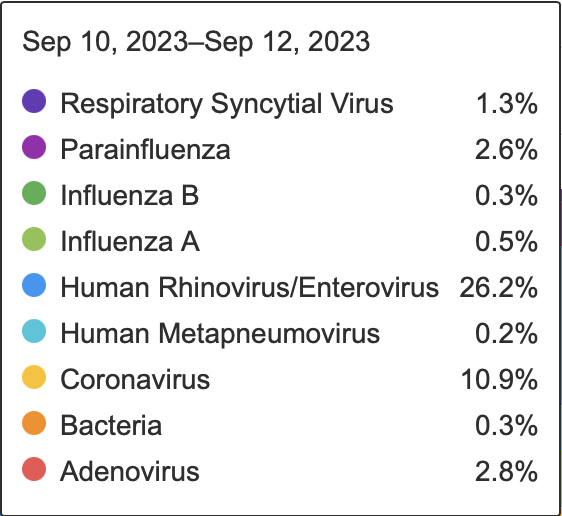
Wastewater surveillance and ED visits/hospitalizations, as well as recent testing data information from Biofire to get a sense of what is going around: the majority of respiratory symptoms right now are due to either Covid-19, Rhinovirus (the common cold) or Enterovirus (a cause of Hand, Foot & Mouth; source).
What variants are around?
We have continued to see mutations in this virus, and there are a few that are particularly noteworthy: “Eris” or EG.5 (read here for more) and BA.2.86. Both show some immune escape, but not to the extent we first feared. In other words, the prior infections and immunizations you’ve already had will still serve as some form of protection — and, even more important, the new vaccines coming out this fall should provide protection.
Should we be masking?
There is likely no clear “right” answer here: the decision needs to be made in the context of what your family’s risk threshold is. What is "right" for my family may not be what is "right" for yours. But a few things to keep in mind:
A recent study showed decreased transmission within households when masking (PMID 37481623). There is value to masks - in the right situation, the pros outweigh the cons.
If any variant turns out to cause more serious illness, or if our family was higher risk, our decision would change - but in my family’s current situation, choosing to mask in some situations but not others makes sense.
We are masking again in higher risk settings (close contact indoor settings, eg airport, crowded grocery stores) but not at school. Here is why:
My kids are up to date on shots, low risk, and we were all infected earlier this year. We already have decent combined immunity.
One of my children goes to a school that requires children to be up to date on all shots including C-19. But even apart from that, they are consistently with the same small group of kids & we are lucky enough to live in an area with high vax rates & thoughtful families who keep their kids home when sick.
It is true that masks can interfere with connection in the classroom. Anyone who says otherwise is not thinking with nuance. But that doesn't mean masks aren't still worth it in some situations.
Not masking at school means we take on a little more risk than we might otherwise. For us, this is a level of risk we're comfortable with (for now).
TPM tip: No matter what you decide, your decision is not set in stone. Be willing to adjust based on what is going on in your household and in your community.
Symptoms to watch for
The most common symptoms in children are:
sore throat
cough*
congestion/runny nose
fever or chills
fatigue
body aches, headache
pink-eye
vomiting and/or diarrhea
Unfortunately, these symptoms overlap with many of the other respiratory illnesses that circulate this time of year — and some overlap with allergies. Given the current wave, my recommendation is to err on the side of caution and test if your child has any of these symptoms, just to make sure you do not inadvertently expose a higher risk person.
Okay, so what to I do if my child tests positive?
As with most other viruses, managing a COVID-19 infection in your child involves supporting them through it and watching for worsening symptoms. Here are the first 3 steps:
Do. Not. Panic. Remember: the good news is that children continue to mostly be at lower risk for these severe outcomes. However, as with other respiratory illnesses, young infants (under age 1) or those with underlying health conditions such as prematurity, heart disease, diabetes, kidney disease, or immunosuppression are at higher risk for worse outcomes.
Touch base with your pediatrician to make sure there are no specific red flags they want you to watch for in your child.
Download my TPM cheat sheet here. This easy to print handout goes over what to do in depth - but in general, your goal is to focus on hydration and comfort, and watch for worsening. What about MIS-C?
What about the new booster vaccine?
Stay tuned for an in-depth post on this soon!